 In April 2022 the Bipartisan Commission on Biodefense released a new report titled The Athena Agenda: Advancing the Apollo Program for Biodefense. Established in 2014, the privately-funded commission convenes periodically and conducts research to assess the state of US biodefense efforts and to make recommendations for change and improvement. Spurred by the events surrounding the COVID-19 pandemic, this report challenges the country to prepare itself for future pandemics by establishing aggressive goals, gathering our “best and brightest” talent, developing action-oriented plans, and funding their accomplishment as the “next Apollo Program.”
In April 2022 the Bipartisan Commission on Biodefense released a new report titled The Athena Agenda: Advancing the Apollo Program for Biodefense. Established in 2014, the privately-funded commission convenes periodically and conducts research to assess the state of US biodefense efforts and to make recommendations for change and improvement. Spurred by the events surrounding the COVID-19 pandemic, this report challenges the country to prepare itself for future pandemics by establishing aggressive goals, gathering our “best and brightest” talent, developing action-oriented plans, and funding their accomplishment as the “next Apollo Program.”
The Commission dubbed this “the Athena Agenda” and included recommendations related to governance and technology, including information technology (IT). The primary IT recommendation is the development of a National Public Health Data System which “…must be able to efficiently integrate, curate, and analyze data in a timely manner from federal, and SLTT public health agencies.” (p. 38) The Commission goes on to say that sustained investment should be brought to bear, building on the initial funding provided by the CARES Act for public health data modernization and the Center for Disease Control and Prevention Data Modernization Initiative (DMI). Once established, according to the report, the National Public Health Data System should focus on data integration and data security/integrity.
 In practical terms the report is not very specific. The US continues to have a very complex public health ecosystem, with IT decisions largely made by state, territorial, local, and tribal (STLT) governments but funded primarily by CDC cooperative agreements. Federal funding can bring with it incentives to work cooperatively, rely on common technical standards, and share data where possible, but it cannot overcome legal or regulatory differences between jurisdictions or perceived differences in needs or priorities.
In practical terms the report is not very specific. The US continues to have a very complex public health ecosystem, with IT decisions largely made by state, territorial, local, and tribal (STLT) governments but funded primarily by CDC cooperative agreements. Federal funding can bring with it incentives to work cooperatively, rely on common technical standards, and share data where possible, but it cannot overcome legal or regulatory differences between jurisdictions or perceived differences in needs or priorities.
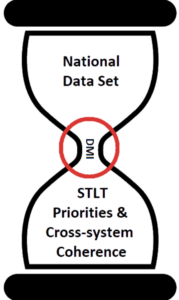
There is an ongoing tension between CDC’s need for building national data sets — usually with de-identified data — and a particular public health agency’s need to improve its data by implementing cross-program integration. DMI may be the bridge between these two priorities, though without adequate funding and workforce it will feel more like an obstacle than an enabler as many activities are “squeezed” through its constrained capacity. STLT public health agencies need to look beyond their strictly parochial interests (sometimes despite pressures to the contrary) and consider their place in the national data fabric. And for its part, CDC needs to be clear about how initiatives that promote a more national view of public health data serves everyone’s needs in the end.
Send us feedback about this blog
