Immunization Information Systems (IIS) are in a precarious position as we come to the end of summer 2024. The urgency of the COVID-19 pandemic is fading, and its funding along with it. The additional funding provided by the Federal government to fight the pandemic cannot be spent after June 30, 2025, which is quickly approaching (though some new funding has just been made available as part of the CDC’s Public Health Infrastructure Grant, or PHIG). Federal budget negotiations for FY25 show an uphill battle between the House and Senate with respect to Health and Human Services (HHS) funding. IIS products are aging just at a time when many agencies are trying to determine a modernized, but sustainable direction.
To help put these many factors into perspective, we have prepared a Force Field Analysis to help describe the state of the country in terms of our ability to provide complete and accessible immunization data via IIS – a key goal of State, Tribal, Local, and Territorial (STLT) health departments.
In the diagram below,
- Driving forces push towards the ideal situation or best possible outcome
- Restraining forces push in the opposite direction towards the worst possible outcome
- Current situation (such as it is) exists because of this equilibrium

The goal is to reduce the number and power of the restraining forces through some mitigating action(s) while increasing the number and power of the driving forces to push to the desired outcome.
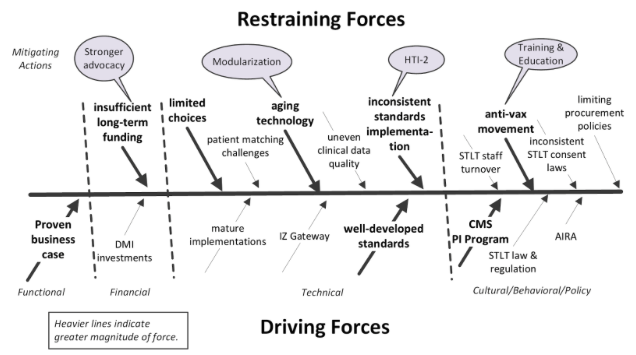
While the Driving Forces may seem compelling, the Restraining Forces can at times be overwhelming. The combined impact of insufficient long-term funding is exacerbated by a COVID “funding cliff;” aging technologies which reduce efficiencies and threaten operations; frustration over inconsistent implementation of technical standards across jurisdictions; and a virulent anti-vax movement and misinformation especially on the Internet. These forces have made it very difficult for IIS projects and immunization programs to maintain their momentum from COVID response.
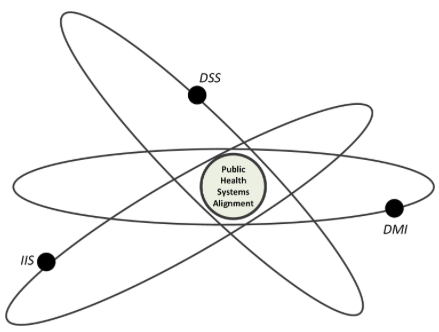
In an even broader public health systems context, it feels like major public health informatics initiatives are struggling to align as a concerted effort.
Just as IIS are struggling to find new, more sustainable solutions, disease surveillance programs are facing the same struggle with their core systems for many of the same reasons. And the Data Modernization Initiative (DMI) does not feel like it is consistently in sync with these two key initiatives; they all feel like they are on their separate but overlapping elliptical orbits around the public health system alignment/coherence goal.
But there are some steps we can take to try to improve the current situation as indicated by the mitigating factors in the force field diagram above:
Stronger advocacy: We need to collectively turn up the heat on Congress to maintain, if not increase, funding for core public health activities and public health informatics projects. We can’t let post-pandemic complacency blind us to the dangers that may lay ahead if we are unprepared for the inevitable next public health emergency. Data management shortcomings and system limitations experienced during COVID-19 can be prevented with prudent investment now.
Modularization of Systems Solutions: Monolithic systems are increasingly difficult to maintain, especially in the face of continually evolving needs. Systems need to be developed in more nimble ways (read Agile) and with a building block architecture (like CDC’s Enterprise Data Analytics and Visualization, or EDAV) that can allow different features and components to evolve more naturally in different ways. The ongoing focus on application programming interfaces (APIs) and system-to-system interoperability makes the case for modular systems even more compelling.
HTI-2: The Health Data, Technology, and Interoperability: Patient Engagement, Information Sharing, and Public Health Interoperability (HTI-2) Proposed Rule has within its provisions, among other things, the alignment of EHR interoperability standards and related technologies with the public health systems with which they interact. While many state-level systems already comply with these standards, a potential Federal rule provides the foundation for other agencies particularly at the local and tribal levels to align more easily as they continue to implement systems.
Training and education: We are all trainers and educators by necessity, and now is the time to continue to write, publish, and speak to whoever will listen about the benefits of public health interventions and the data systems that support these activities.
