 In August, 2024 the Sequoia Project released the first formal version of the Exchange Purpose (XP) Implementation SOP for Public Health. This document provides the essential information to Qualified Health Information Networks (QHINs) for how to apply the standard QHIN Technical Framework (QTF) specifically to public health transactions supported by TEFCA.
In August, 2024 the Sequoia Project released the first formal version of the Exchange Purpose (XP) Implementation SOP for Public Health. This document provides the essential information to Qualified Health Information Networks (QHINs) for how to apply the standard QHIN Technical Framework (QTF) specifically to public health transactions supported by TEFCA.
The SOP document provides the necessary message header and coding information for IHE and FHIR transactions sent using the TEFCA network. Core transactions are defined for both message delivery (“push”) as well as query, and facilitated FHIR-based message delivery and query are also covered. Two specific use case definitions are provided: for electronic lab reporting (ELR) and electronic case reporting (eCR), but only message delivery is defined for use and not message query (either via IHE standards or FHIR). This is different from the draft SOP which proposed support for electronic case investigation query from public health as well. The SOP seems to say that other use cases can be implemented on the TEFCA network as long as public health (and not clinical care) initiates them. So, this would allow other useful public health transactions to take place over the network.
Several public health agencies have stepped forward and begun TEFCA-based interoperability projects in late 2023, including the Washington State and Alaska (eICR submission via the eHealth Exchange), and Fairfax County, Virginia and Southern Nevada (eCR case investigation via FHIR-based query). While others will likely follow, many public health agencies still have lots of questions about the “why,” “how,” and “how much” of TEFCA implementation. In July 2024, the Association of State and Territorial Health Officers (ASTHO) published a useful frequently asked questions document with ASTP/ONC’s help to try to answer some of these common questions.
To help put these many factors into perspective, we have prepared a Force Field Analysis to help describe how public health agencies think about TEFCA participation today. In the diagram below,
- Driving forces push towards the ideal situation or best possible outcome
- Restraining forces push in the opposite direction towards the worst possible outcome
- The current situation (such as it is) exists because of this equilibrium
The goal is to reduce the number and power of the restraining forces through some mitigating action(s) while increasing the number and power of the driving forces to push to the desired outcome.
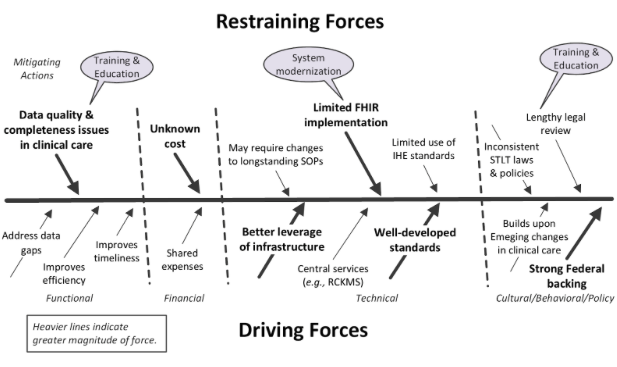
The key driving forces pushing in favor of TEFCA deployment in public health are the potential for better leverage of shared technical infrastructure across an agency; the existence of well-developed technical standards to support TEFCA-based interoperability; and strong and consistent Federal backing through both ASTP/ONC and CDC. Key restraining forces include data quality issues within clinical care (will the new interfaces be worth the effort?); the unknown cost of participation in TEFCA; and limited implementation of new standards like HL7’s Fast Healthcare Interoperability Resources (FHIR) in public health. Over time, primarily through training, education, and system modernization, these restraining forces should be mitigated.
As is often the case, agencies are watching the early adopters and tracking their successes and problems. For public health, the success of TEFCA will be tied more to the success of FHIR over the next few years than almost anything else. As the use of FHIR-based interfaces increases in clinical care, concomitant improvements in data quality will only strengthen the case for TEFCA in public health.
